This post delves into the pathogenesis, epidemiology, and prevention strategies of Staphylococcus aureus, a common yet dangerous bacterium that can cause severe human infections. It emphasizes the importance of understanding its unique morphology, disease causes, diagnosis, and treatment methods for effective outbreak management.
Staphylococci are grape-like clusters of small, spherical cells (1μL each). Staphylococci are bacteria that produce catalase but are not motile. There are about 30 species and subspecies in the Staphylococcus genus. The table below outlines the most relevant aspects in a medical context. S. aureus (and E. coli) are among the most common organisms that cause bacterial infections in humans.
An overview of the most common Staphylococcus species that affect humans.
| Species | Parameter |
| S. aureus | Coagulase-positive; colonies golden yellow. Local purulent Infections: furuncles, carbuncles, bullous impetigo, wound infections, sinusitis, otitis media, mastitis puerperalis, ostitis, postinfluenza pneumonia, sepsis. Toxin-caused illnesses: food Poisoning, dermatitis exfoliativa, toxic shock syndrome. |
| S. epidermidis | Coagulase-negative; sensitive to novobiocin; most frequent CNS* pathogen; opportunist; infection requires host predisposition; foreign body infections with discrete clinical symptoms |
| S. saprophyticus | Coagulase-negative; resistant to novobiocin. Urinary tract infections in young women (10–20%); occasional nonspecific urethritis in men |
* CNS: coagulase-negative staphylococci
Staphylococcus Aureus
Morphology and culturing
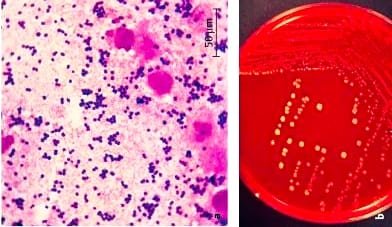
Figure (a) illustrates the appearance of Gram-stained S. aureus. This facultative anaerobe is easily grown on standard nutrient mediums at 37°C. After 24 hours of incubation, colonies form as shown in Figure (b). Hemolytic zones are frequently seen surrounding the colonies.
Fine structure (Cell Wall Structure and Function)
- Cell wall is composed of a thick murein layer.
- Linear teichoic acids and polysaccharides are covalently coupled to the murein polysaccharide.
- Lipoteichoic acids anchor in the cell membrane, triggering complement activation and macrophage cytokine secretion.
- Cell wall-associated proteins, including Clumping factor, fibronectin-binding protein, and collagen-binding protein, bind to specific fibrinogen, fibronectin, and collagen.
- Protein A binds to the Fc portion of immunoglobulins, preventing correct opsonizing antibody binding and hindering phagocytosis.
Extracellular toxins and enzymes
S. aureus produces numerous enzymes and toxins that, along with fine structures, determine the pathogenesis of infections, with the most crucial ones being:
Plasma coagulase
The enzyme functions similarly to thrombin, converting fibrinogen into fibrin, making tissue microcolonies surrounded by fibrin walls challenging to phagocytose.
alpha-toxin
The substance can cause severe CNS effects, damage membranes, leading to hemolysis, and is linked to a form of dermonecrosis.
Leukocidin
Degranulation is a process that damages both microphages and macrophages.
Exfoliatins
Are responsible for a form of epidermolysis.
Food poisoning symptoms can be caused by eight serologically differentiated enterotoxins, which are superantigens and cannot be inactivated by heating to 100 8C for 15-30 minutes.
Toxic shock syndrome toxin-1 (TSST-1)
TSST-1, a superantigen produced by 1% of Staphylococcus strains, triggers clonal expansion of 10% T lymphocyte types, causing massive cytokine production and toxic shock symptoms.
Pathogenesis of Staphylococcus aureus
S. aureus infections can be categorized into three distinct courses of pathogenesis and symptoms.
Invasive infections
- Pathogens remain in situ after penetrating derma or mucosa.
- Causes local infections characterized by purulence.
- Examples include furuncles, carbuncles, wound infections, sinusitis, otitis media, and mastitis puerperalis.
- Postoperative/posttraumatic otitis/osteomyelitis.
- Endocarditis post-heart surgery.
- Post influenza pneumonia.
- Sepsis in immunocompromised patients.
- S. aureus and E. coli cause nearly half of inpatient sepsis cases.
S. aureus can colonize inert foreign bodies by binding staphylococci to fibrinogen or fibronectin, creating a biofilm that may serve as an infection focus.

Figure 1 Furuncles
Toxicoses
Food poisoning is a condition resulting from consuming enterotoxins, causing symptoms such as nausea, vomiting, and diarrhea within hours of ingestion.
Mixed forms
Dermatitis exfoliativa, pemphigus neonatorum, and bullous impetigo are caused by exfoliatin-producing strains, while Toxic shock syndrome (TSS) is caused by TSST-1 strains, causing hypotension, fever, and a scarlatiniform rash.
Diagnosis of Staphylococcus aureus
Pathogen identification involves microscopic and culture-based methods, distinguishing S. aureus from coagulase-negative species through plasma coagulase and clumping factor, and detecting enterotoxins and TSST-1 using immunological and molecular biological methods.
Treatment of Staphylococcus aureus
Antibiotics, including penicillinase-resistant penicillins, are the preferred treatment for severe infections due to their effectiveness against methicillin-resistant strains, which also applies to all betalactams.
Epidemiology and prevention
S. aureus is a common skin and mucosa colonizer, with high carrier rates (up to 80%) among hospital patients and staff, primarily in the anterior nasal mucosa area, where it can spread to susceptible individuals.
S. aureus is a common cause of nosocomial infections, with certain strains causing hospital epidemics. Identifying the epidemic strain requires differentiation of relevant infection isolates from other strains, with molecular methods becoming more common.
Washing hands thoroughly before medical procedures is crucial in hospitals, and intranasal application of antibiotics like mupirocin can reduce bacterial counts in carriers.
CNS are essential components of human skin and mucosa flora, acting as classic opportunists that only cause infections based on a specific host’s disposition.
S. epidermidis
CNS infections are primarily caused by foreign body infections, such as catheters, endoprostheses, and cardiac pacemakers. These infections develop when foreign bodies are covered by matrix proteins, allowing staphylococci to bind and proliferate on the surface. The resulting biofilm, protected by antibiotics and the immune system, can become infection foci, allowing the CNS to enter the bloodstream and cause sepsis-like illnesses. Removal of the foreign body is often necessary to prevent further complications.
S. saprophyticus
S. hemolyticus is responsible for 10-20% of acute urinary tract infections, particularly dysuria in young women, and a small proportion of nonspecific urethritis in sexually active men, making antibiotic treatment problematic due to multiple resistance.
Conclusion
Staphylococcus aureus is a significant bacteria with a unique shape and potential for serious infections. Understanding its pathogenesis, diagnosis, and treatment is crucial for managing its impact on health. Preventative measures, such as good hygiene and awareness of its spread, help reduce infections. Staying informed and proactive is the first step to prevention against this dangerous bacteria.