Crimean-Congo Hemorrhagic Fever Virus (CCHFV) is a tick-borne virus with high virulence that leads to a severe zoonotic disease referred to as Crimean-Congo Hemorrhagic Fever (CCHF). Being a recognized important public health problem, particularly in the African, Asian, Eastern European, and Middle Eastern regions, CCHFV is challenging because of its high mortality rate and risk of hospital-acquired outbreaks.
This lecture aims to provide an overview of CCHFV, its virology, epidemiology, transmission, clinical features, diagnosis, treatment, and prevention. It is aimed at medical students, health professionals, and researchers with emphasis on simplicity, humanized text, and recallable facts.
1. Virology of Crimean-Congo Hemorrhagic Fever Virus
1.1. Classification and Organization
- Family: Bunyaviridae (now in Orthonairoviruses)
- Genus: Nairovirus
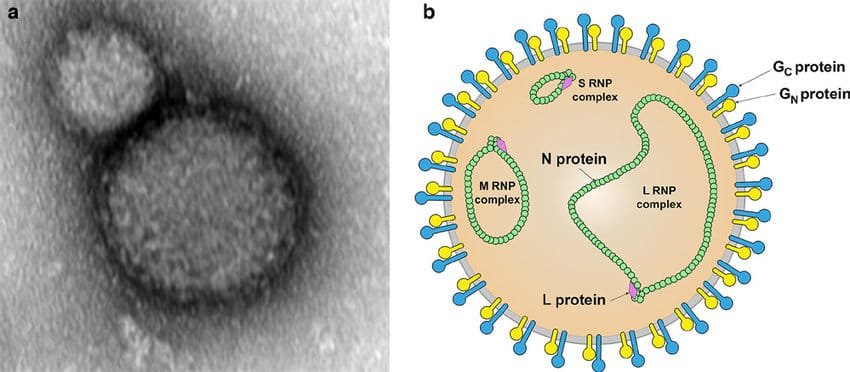
- Type of Virus: Enveloped, single-stranded, negative-sense RNA virus
- Form: Pleomorphic, spherical particles (~100 nm diameter)
- Genomic Segments: Three segments — Small (S), Medium (M), and Large (L)
Minimal requirements for commemoration:
The genome of the virus consists of three pieces of negative-sense RNA, akin to a three-part puzzle that codes for all the proteins required for replication and virulence.
1.2. Genetic Material and Viral Proteins of Crimean-Congo Hemorrhagic Fever
- S segment: Codes for nucleoprotein (NP)
- M segment: Codes glycoproteins (Gn and Gc) involved in attachment and entry
- L segment: Encodes RNA-dependent RNA polymerase.
1.3. Structural Elements
- Envelope: Lipid bilayer from host cell membranes
- Surface glycoproteins: Permit attachment to host cells.
- Nucleocapsid: Houses the viral RNA.
2. Epidemiology and Geographic Distribution
2.1. Worldwide Dispersion
- Native to Africa, Asia, Eastern Europe, Middle East
- Outbreaks have been reported in Sudan, Iran, Turkey, Pakistan, Russia, and Africa
2.2. Reservoirs and Vectors
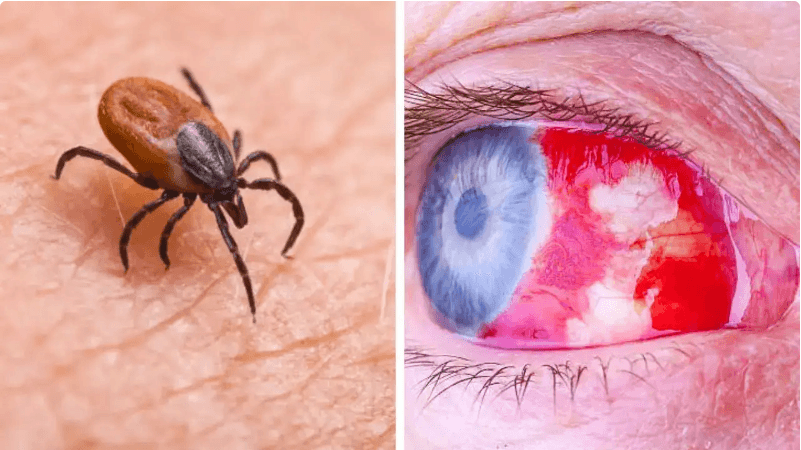
- Primary reservoir: Hard ticks (family Ixodidae), especially Hyalomma spp.
- Amplifying hosts: Domestic animals like bovines, ovines, and caprines.
- Humans: Accidental hosts, infected by the bites of ticks or contact with blood/tissues of infected animals
Remember:
- “Ticks are the natural reservoirs, and humans are incidental hosts, somewhat like passengers who get trapped in a storm they did not create.
3. Transmission Dynamics
3.1. Tick-Borne Transmission
- Hyalomma ticks spread the virus upon feeding
- The virus can be passed on by ticks transstadially (via life cycles) and transovarially (female tick to eggs)
3.2. Human-to-Human Transmission
Occurs via:
- Coming in contact with the blood, tissues, or body fluids of infected patients
- Nosocomial (hospital-acquired) transmission, especially in health care facilities with inadequate protective precautions
3.3. Alternative Pathways
Rarely through:
- Lab accidents
- Blood transfusions
Chief Consideration:
Although the main vector is ticks, human infection is mostly through contact with infected tissues or blood, making it essential to use protective measures.
4. Clinical Features of Crimean-Congo Hemorrhagic Fever

4.1. Incubation Period
- Typically 1–13 days following exposure
4.2. Stages of Illness
| Stage | Characteristics |
|---|---|
| Incubation Period | Usually asymptomatic; varies depending on transmission mode and received dosage |
| Acute febrile phase | Abrupt high fever, intense headache, muscle ache, malaise, vomiting, diarrhea |
| Hemorrhagic phase | The development of petechiae, ecchymoses, mucous membrane bleeding, gingival bleeding, and hematuria |
| Recovery or death | Recovery is possible after 2-3 weeks; high mortality (~10-40%) if left untreated |
4.3. Pathogenesis
- Virus infects endothelial cells, causing vascular damage
- Cytokine storm leads to increased vascular permeability
- Hemorrhage is due to coagulation defects and vascular fragility
Notable observation:
- “The virus’s assault on blood vessels transforms the body’s own defenses into a battleground of bleeding.
5. Diagnosis of CCHFV Infection
5.1. Laboratory Tests
| Test | Timing | Description |
|---|---|---|
| RT-PCR | Initial stage | Detects viral RNA; is the gold standard for early detection |
| ELISA (Immunoglobulin M and Immunoglobulin G) | After an interval of 4 to 7 days | Detects specific antibodies; if IgM is present, then the infection is recent |
| Virus isolation | Seldom performed | Needs biosafety level 4 laboratories |
| Complete Blood Count (CBC) | Supportive Care | Leukopenia and thrombocytopenia |
| Coagulation profile | Supportive | DIC indicators, prolonged PT/PTT |
5.2. Biosafety Considerations
- BSL-4 containment is needed for laboratory work because of high infectivity
6. Management and Treatment
6.1. Supportive Care
- Stay hydrated
- Correct coagulopathies
- Manage bleeding and organ failure
6.2. Antiviral Treatment
- Ribavirin has been partially effective; if administered early
- No specific approved antiviral; supportive care is mainstay
6.3. Infection Control
- Proper PPE use
- The separation of verified instances. – Disposal of contaminated materials safely
7. Prevention and Control
7.1. Personal Safety Measures
- Wear protective attire when in tick-infested areas
- Use insect repellents.
- Avoid contact with blood or body fluids of infected animals or persons
7.2. Control Measures for Ticks
- Spray acaricides on the animals
- Environmental management to reduce tick habitats
7.3. Immunization
- No human vaccine widely available yet
- Vaccines are under investigation, mostly in animal health
7.4. Public Health Measures
- Surveillance of outbreaks
- Increasing awareness among populations at risk
- Strict biosafety measures in clinical environments
8. Summary and Key Points for Remembering
- CCHFV is a lethal, tick-borne virus causing hemorrhagic fever with high mortality.
- Primarily transmission by Hyalomma ticks; transmission to humans occurs by tick bites or contact with infected blood/tissues.
- Clinical characteristic: Acute fever, hemorrhages, and high mortality if left untreated.
- Diagnosis: RT-PCR and serology are most significant; diagnosis should be done early.
- Treatment: Antiviral supportive therapy with medications like ribavirin; prevention involves tick control and protective measures.
- Infection control: Essential in healthcare environments to avoid hospital-acquired infections.
9. Citations and Additional Literature 1.
- World Health Organization (WHO). Crimean-Congo Hemorrhagic Fever Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/crimean-congo-haemorrhagic-fever
- Fooks, A. R., et al. “Crimean-Congo Hemorrhagic Fever Virus.” Virology, 2018*.
- Bente, D. A., et al. *”Crimean-Congo Hemorrhagic Fever: History, Epidemiology, Pathogenesis, and Vaccines.”* Antiviral Research, 2019*.
- Laboratory Biosafety Manual, 4th Edition. World Health Organization. 5. WHO. Clinical management of severe viral hemorrhagic fever. https://www.who.int/csr/resources/publications/WHO_CDS_CSR_GAR_2008_1/en/ —