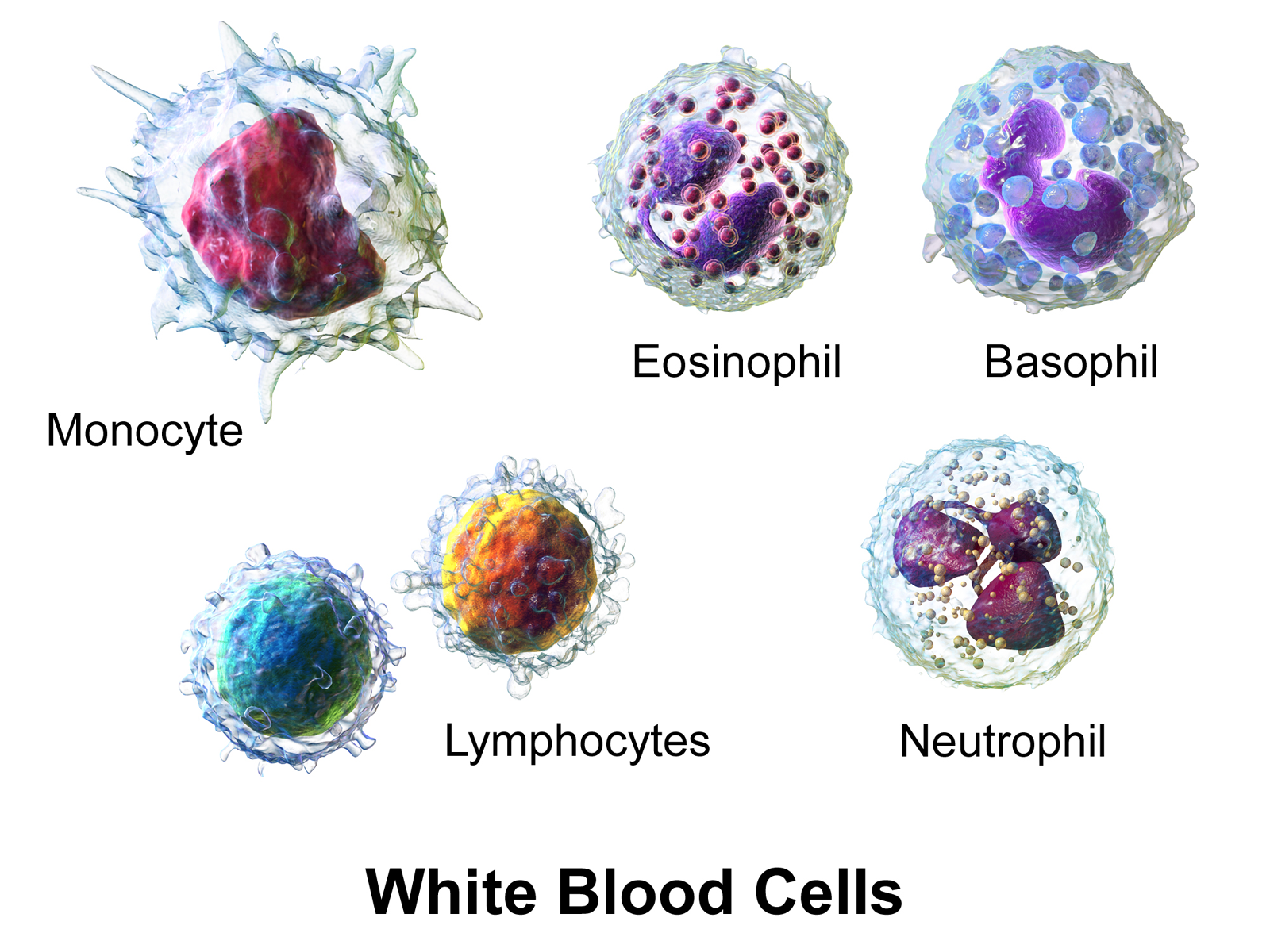
Imagine your body as a highly sophisticated fortress, constantly on alert against invaders like bacteria, viruses, fungi, and parasites. The cellular defense mechanisms are the soldiers and defenses that protect you from disease, ensuring your body’s integrity and health. These defenses involve a variety of specialized cells, primarily white blood cells (leukocytes), each with unique roles in defending against infections and maintaining immune surveillance.
In this article, we will explore the five main types of leukocytes—neutrophils, eosinophils, basophils, monocytes, and lymphocytes—and their roles in natural (innate) and acquired (adaptive) immunity. We will also delve into how these cells participate in processes like phagocytosis, inflammation, and immune regulation—making this an essential resource for medical laboratory students and healthcare professionals.
The Principal Leukocytes in Peripheral Blood
Your blood contains a diverse cast of immune cells, each with specialized functions:
- Neutrophils
- Eosinophils
- Basophils
- Monocytes
- Lymphocytes
Some of these cells participate directly in phagocytosis—the process of engulfing and destroying pathogens—while others, like lymphocytes, are central to adaptive immunity.
Question for reflection:
Can you think of how these different leukocytes coordinate during an infection? Which cells are first responders, and which are responsible for long-term immunity?
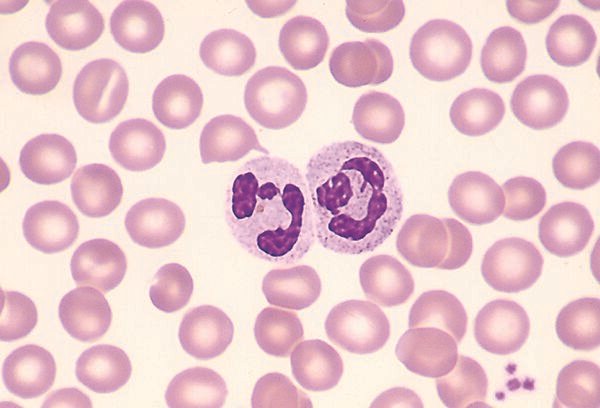
Neutrophils: The Body’s First Line of Defense
What are neutrophils?
Neutrophils, also called polymorphonuclear leukocytes (PMNs), are the most abundant white blood cells in your blood, making up approximately 50-70% of circulating leukocytes. They are your body’s rapid responders to infection.
Physical Characteristics:
- Diameter: 10-15 μm
- Nucleus: multi-lobed (2-5 lobes)
- Cytoplasm: filled with neutral-staining granules
Granules and Their Contents:
Neutrophils contain granules that store enzymes and proteins essential for killing microbes:
- Primary (azurophilic) granules: contain enzymes like myeloperoxidase, elastase, lysozyme, and defensins—all crucial for destroying bacteria.
- Secondary granules: include lactoferrin, collagenase, and NADPH oxidase components.
- Tertiary granules: contain gelatinase and plasminogen activator, aiding tissue remodeling.
Lifecycle and Movement:
- Marginating pool: about half of neutrophils adhere loosely to blood vessel walls, ready to migrate.
- Circulating pool: the rest circulate freely in the blood for about 6-10 hours.
- Diapedesis: neutrophils migrate through blood vessel walls into tissues in response to infection or injury, guided by selectins and chemotactic factors.
Chemotactic Factors Attracting Neutrophils:
- Complement components (like C3a, C5a)
- Bacterial products
- Platelet activating factor
- Cytokines from lymphocytes and macrophages
Phagocytosis by Neutrophils:
Once in tissues, neutrophils engulf pathogens in a process called phagocytosis. They form a phagosome, which fuses with granules to create a phagolysosome, where enzymes and reactive oxygen species (ROS) kill the invader.
Respiratory (Oxidative) Burst:
This process involves increased oxygen consumption, producing superoxide radicals and hydrogen peroxide, which are toxic to microbes. The enzyme NADPH oxidase plays a central role; its deficiency leads to chronic granulomatous disease—a condition with recurrent infections.
Prompting question:
Can you explain how the respiratory burst enhances microbial killing in neutrophils?
Eosinophils: The Parasite and Allergy Fighters
What are eosinophils?
Eosinophils are smaller than neutrophils, about 12-15 μm, and comprise 1-3% of circulating leukocytes in healthy individuals. They are especially important in combating parasitic infections and allergic responses.
Physical Features:
- Bilobed or elliptical nucleus, often eccentrically located
- Cytoplasm filled with large, orange-reddish granules that stain with eosin dye
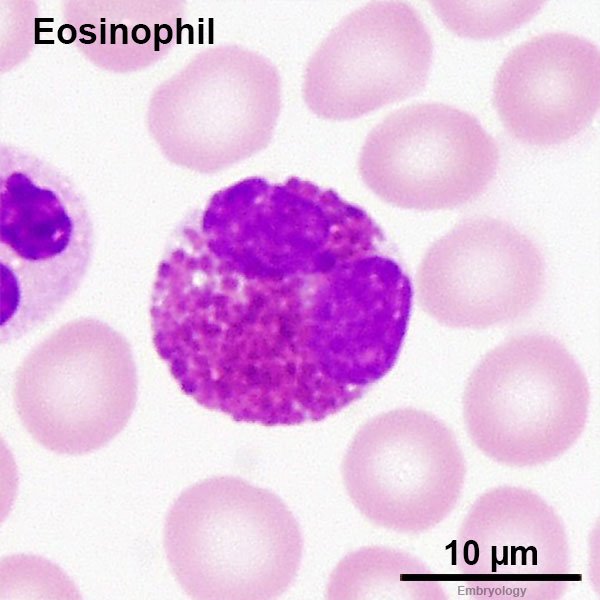
Granule Contents:
- Major Basic Protein (MBP)
- Eosinophil Cationic Protein (ECP)
- Eosinophil Peroxidase
- Neurotoxins
Functions:
While capable of phagocytosis, eosinophils are less efficient than neutrophils. Their main roles include:
- Neutralizing products released by basophils and mast cells during allergic reactions
- Killing parasitic worms (helminths) by releasing granule contents
Question:
How do eosinophils contribute to allergic reactions, and why are they increased during parasitic infections?
Basophils and Mast Cells: Mediators of Allergic Responses
Basophils:
- Represent less than 1% of circulating white blood cells
- Diameter: 10-15 μm
- Have deep-blue, coarse granules containing histamine, heparin, and eosinophil chemotactic factor
- Play a key role in immediate hypersensitivity reactions by releasing granule contents upon allergen contact, especially when IgE antibodies are involved
Mast Cells:
- Reside in tissues (e.g., skin, mucous membranes) and resemble basophils but are larger and live longer (9-18 months)
- Contain similar granules with enzymes like acid and alkaline phosphatases and proteases
- Central in allergic responses by releasing histamine and other mediators upon allergen exposure
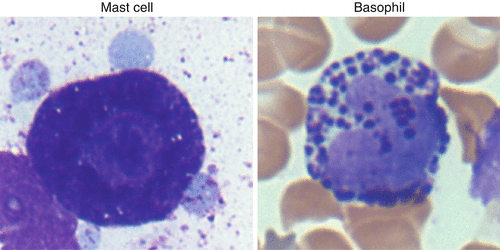
What is the significance of IgE binding to basophils and mast cells in allergy development?
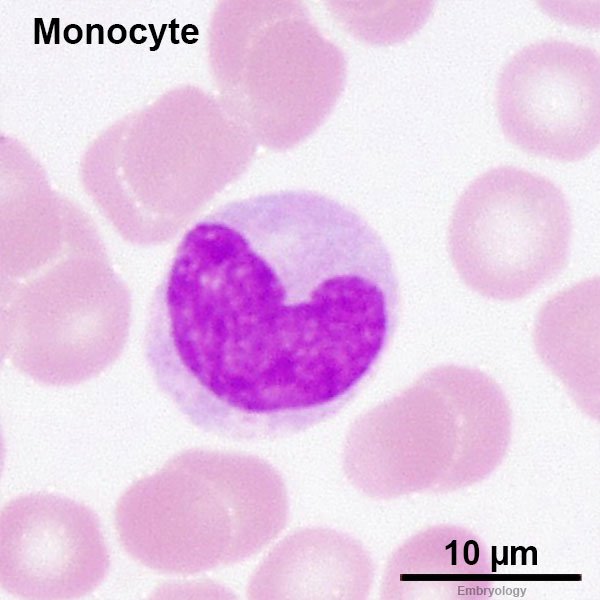
Monocytes: The Precursors to Tissue Macrophages
What are monocytes?
Large cells (~12-22 μm), with a distinctive horseshoe-shaped nucleus and grayish-blue cytoplasm containing lysosomal-like granules.
Lifecycle and Transition:
- Circulate in the blood for up to 70 hours
- Migrate into tissues where they differentiate into macrophages (e.g., alveolar macrophages in lungs, Kupffer cells in liver)
Functions in Tissues:
- Phagocytosis of pathogens and debris
- Secretion of cytokines and mediators
- Antigen presentation to T lymphocytes
- Tumor and parasite destruction
Differences from Monocytes:
Macrophages are larger, longer-lived, and more phagocytically active, often residing in tissues for months.
Prompt:
Why is the monocyte-macrophage system vital for both innate and adaptive immunity?
Dendritic Cells: The Antigen Presenters
What are dendritic cells?
Named for their branched, dendrite-like extensions, these cells are the key link between innate and adaptive immunity.
Main Functions:
- Phagocytosing antigens in tissues
- Migrating to lymphoid organs
- Presenting processed antigens to helper T cells to initiate immune responses
Locations:
- Langerhans cells in the skin and mucous membranes
- Interstitial dendritic cells in organs like the lungs and liver
- Interdigitating dendritic cells in lymphoid tissues
Reflection:
How do dendritic cells orchestrate the transition from innate to acquired immunity?
Toll-Like Receptors (TLRs): The Innate Immune Sensors
Recent discoveries have highlighted Toll-like receptors (TLRs) as crucial for pathogen recognition. These receptors are present on monocytes, macrophages, and neutrophils.
How do TLRs work?
- Recognize specific microbial components (called ligands) such as lipoteichoic acid, peptidoglycan, or lipopolysaccharide (LPS)
- Trigger phagocytosis and cytokine production, amplifying immune responses
Examples:
- TLR2: detects gram-positive bacterial components
- TLR4: recognizes LPS from gram-negative bacteria
Question:
Why are TLRs considered the body’s early warning system against infection?
The Process of Phagocytosis: How Cells Destroy Invaders
Phagocytosis is the cellular process of engulfing pathogens and debris, essential for innate immunity.
Four Main Steps:
- Adherence: The phagocyte attaches to the microbe, aided by opsonins like antibodies or complement proteins that coat the pathogen.
- Engulfment: Cytoplasm extends around the microbe, forming a phagosome.
- Phagolysosome Formation: The phagosome fuses with lysosomes, releasing enzymes and ROS to kill and digest the microbe.
- Exocytosis: Indigestible debris are expelled from the cell.
Oxygen-Dependent Killing:
The respiratory burst produces superoxide radicals and hydrogen peroxide, which are highly toxic to microbes. Enzymes like myeloperoxidase generate hypochlorite (bleach-like substances), enhancing killing efficiency.
Prompt:
What might happen if NADPH oxidase is defective? How does this impact microbial killing?
Inflammation: The Body’s Response to Injury and Infection
What is inflammation?
It’s the body’s complex response to injury or infection, involving increased blood flow, capillary permeability, and immune cell migration.
Key Features:
- Redness, swelling, heat, pain
- Increased blood supply (vasodilation)
- Leakage of plasma into tissues (edema)
- Recruitment of neutrophils and macrophages
Sequence of Events:
- Release of chemical mediators like histamine from mast cells causes vasodilation.
- Endothelial cells retract, increasing permeability.
- Neutrophils adhere to vessel walls via selectins and migrate into tissues (diapedesis).
- Chemotactic factors guide neutrophils to the injury site.
- Neutrophils and macrophages perform phagocytosis, clearing pathogens and debris.
Chronic Inflammation
When inflammation persists, tissue damage may occur, involving lymphocytes and long-term immune responses.
Reflective question:
How does understanding the inflammatory process assist in interpreting laboratory test results, such as elevated CRP levels?
Summary: The Role of Cellular Defense in Immunity
The immune system’s cellular defenses are a marvel of biological engineering. From rapid neutrophil responses to long-lived macrophages and the antigen-presenting prowess of dendritic cells, each component plays a vital role. Innate immunity provides immediate, nonspecific defense, with phagocytosis and inflammation as the main pillars. Meanwhile, other cells like lymphocytes and specialized receptors (like TLRs) set the stage for specific, long-lasting immunity.
Final thought:
Understanding these mechanisms is crucial for anyone working in medical laboratories or healthcare, as they underpin diagnostic markers, treatment strategies, and vaccine development.
References and Further Reading
- Harmening, D. (2002). Clinical Hematology and Fundamentals of Hemostasis. F. A. Davis.
- Abbas, A. K., Lichtman, A. H., & Pillai, S. (2019). Cellular and Molecular Immunology. Elsevier.
- Janeway, C., et al. (2005). Immunobiology: The Immune System in Health and Disease. Garland Science.
- Kumar, V., Abbas, A. K., & Aster, J. C. (2018). Robbins Basic Pathology. Elsevier.
- MedlinePlus. (n.d.). White blood cells. National Library of Medicine.
Remember:
Reflect on how each cell and process contributes to your body’s defense. The more you understand, the better you’ll grasp the complex, beautiful system that keeps us healthy!