Picture your body as a well-run city. When all’s well, all systems work together in harmony. But when there’s an invasion—let’s say a bacterial infection or injury to tissue—your body must react swiftly to defend and repair itself. One of its initial reactions is the release of acute-phase reactants. Special proteins, these reactants surge in the blood rapidly during inflammation or tissue injury. It’s essential that medical laboratory students and healthcare personnel know about these reactants since they’re important indicators of inflammation, infection, or tissue injury.
In this essay, we will cover what acute-phase reactants are, their functions, how they respond to various stimuli, and their significance in clinical diagnosis. We will particularly cover major proteins like C-reactive protein (CRP), serum amyloid A, complement components, and others, and outline their functions in health and disease.
What Are Acute-Phase Reactants?
Definition:
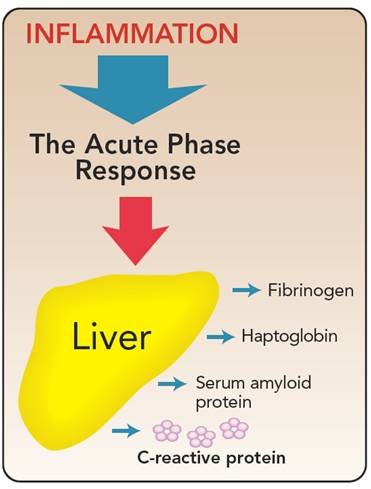
Acute-phase reactants are serum components—primarily proteins—that rise in concentration by at least 25% from their normal values during acute inflammation, infection, trauma, or tissue damage. They are effectively part of the body’s immediate reaction to injury or invasion, serving to localize damage, combat infecting agents, and initiate repair.
Key Features:
- Made mostly by the liver (hepatocytes).
- Their levels can rise several-fold within 12 to 24 hours after an inflammatory stimulus.
- The extent of rise varies with different reactants.
- They are mediated in their response by cytokines—chemical messengers such as interleukin-6 (IL-6), IL-1β, and tumor necrosis factor-alpha (TNF-α)—released from immune cells such as monocytes and macrophages in areas of inflammation.
Reflective Question:
Can you imagine how knowing these proteins would assist a physician in identifying if a patient has a current infection or inflammation?
Major Types of Acute-Phase Reactants and Their Roles
Let us discuss some of the most significant acute-phase proteins, their functions, and what their levels signify.
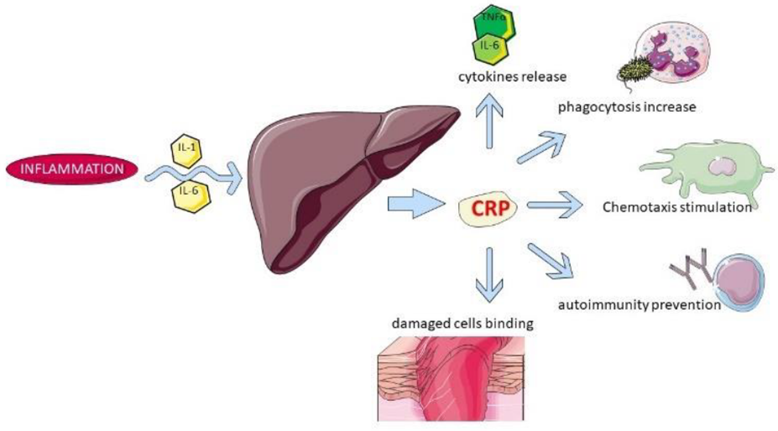
1. C-Reactive Protein (CRP)
CRP is the most recognized acute-phase reactant. It was once believed to be an antibody to pneumococcal bacteria but was subsequently identified as a general marker of inflammation.
Response Time and Magnitude:
- Increases steeply within 4-6 hours following an inflammatory stimulus.
- Levels can increase dramatically, sometimes up to a thousandfold, peaking within 48 hours.
- Decreases just as rapidly once the stimulus is withdrawn.
Normal and Elevated Levels:
- Normal values are low, usually 1.5 mg/L in men and 2.5 mg/L in women.
- Raised CRP (>10 mg/L) indicates active inflammation or infection.
Structure and Function:
CRP is a pentameric protein (five subunits bound noncovalently) with a molecular weight of around 118,000 daltons. CRP behaves like a primitive antibody by:
- Opsonizing microbes (coating pathogens to make phagocytosis easier).
- Activation of the complement system through the classical pathway.
- Binding to phosphocholine within microbial membranes, facilitating immune defense.
Clinical Significance:
As CRP levels rise and fall quickly, it’s a helpful marker for monitoring disease activity as well as response to treatment. Decreasing CRP levels, for example, may indicate that an infection has been treated successfully.
Example:
A patient with bacterial pneumonia will have elevated CRP. Its decrease is monitored to see if the infection is resolving.
Prompt for Reflection:
Why is CRP a better marker of acute inflammation than other proteins that have slower responses?
2. Serum Amyloid A (SAA)
SAA is another major acute-phase protein with the same response as CRP, increasing as much as a thousandfold during inflammation.
Function:
- It is associated with HDL cholesterol in plasma.
- Participates in the metabolism of cholesterol, particularly in the removal of excess cholesterol from macrophages in injured areas.
- Contributes to tissue cleanup during inflammation.
Clinical Relevance:
- Elevated SAA levels are more evident in bacterial infections.
- Chronic elevation of SAA levels can lead to amyloidosis, a disease characterized by abnormal tissue deposition of amyloid proteins.
Example:
In bacterial sepsis, SAA levels can skyrocket, signaling severe systemic inflammation.
Question:
How would the increase in SAA influence amyloid deposit formation in chronic inflammatory diseases?
3. Complement System
Complement proteins are a collection of serum enzymes that amplify immune responses, including opsonization, inflammation, and cell lysis.
Principal Functions:
- Opsonization: Tagging pathogens for elimination.
- Chemotaxis: Attracting immune cells to the infected area.
- Cell lysis: Destroying bacteria or infected cells.
Activation Pathways:
- Classical pathway: Activated by antibody-antigen complexes.
- Alternative pathway: Activated directly by microbial surfaces.
Clinical Note:
Alterations in complement levels may reflect immune activation or deficiencies.
4. Mannose-Binding Lectin (MBL)
MBL, or mannose-binding protein, binds to certain sugars on microbes, particularly bacteria, fungi, and certain parasite
Function:
- Acts as an opsonin.
- Activates the complement system via the lectin pathway.
Clinical Relevance:
Low MBL levels can predispose someone to recurrent infections, most notably yeast infections.
5. Alpha-1-Antitrypsin (AAT)
AAT is a protease inhibitor that primarily inhibits elastase, which is an enzyme secreted by neutrophils.
Role in Health:
- Safeguards lung tissue against injury during inflammation.
- Controls cytokine production.
Deficiency and Disease:
- Deficiency in AAT can result in premature emphysema, particularly in smokers.
- Homozygous forms may cause liver disease, cirrhosis, or hepatitis.
Example:
A patient with AAT deficiency might develop emphysema despite not being a smoker, emphasizing the importance of this reactant in lung health.
6. Haptoglobin
Haptoglobin binds free hemoglobin released during intravascular hemolysis, thus preventing iron loss and oxidative injury.
Response to Inflammation:
- Levels rise during inflammation.
- However, during hemolysis, the levels may initially decrease due to consumption.
Clinical Use: – Increased haptoglobin indicates inflammation.
- Low levels may signal hemolytic anemia.
7. Fibrinogen
Fibrinogen is both an acute-phase protein and a clotting factor.
Function:
- Converts to fibrin to create blood clots.
- Increases red blood cell aggregation, which can influence blood viscosity.
Clinical Relevance:
- Increased fibrinogen is linked with heightened cardiovascular disease risk, including coronary artery disease.
8. Ceruloplasmin
Ceruloplasmin is a copper-transporting protein.
Function:
- Transports copper in the blood.
- Acts as a ferroxidase, oxidizing iron to a form that can bind to transferrin for transport.
Clinical Significance:
- Low levels are typical of Wilson’s disease, an inherited condition causing copper buildup in tissues.
Summary Table of Major Acute-Phase Reactants
| Protein | Normal Response Time | Typical Concentration Range | Main Function |
|---|---|---|---|
| CRP | 4–6 hours | 0.5–10 mg/dL | Opsonization, complement activation |
| Serum Amyloid A | 24 hours | ~30 µg/mL | Cholesterol removal, inflammation modulation |
| Alpha-1-Antitrypsin | 24 hours | 200–400 mg/dL | Protease inhibition |
| Fibrinogen | 24 hours | 110–400 mg/dL | Clot formation, wound healing |
| Haptoglobin | 24 hours | 40–200 mg/dL | Hemoglobin binding, antioxidant activity |
| Ceruloplasmin | 48–72 hours | 20–40 mg/dL | Copper transport, iron oxidation |
| Complement C3 | 48–72 hours | 60–140 mg/dL | Immune response facilitation |
| Mannose-binding protein | Variable | 0.15–1.0 µg/mL | Microbial recognition, complement activation |
Why Are Acute-Phase Reactants Important?
These proteins can be understood and quantified to gain valuable knowledge of an individual’s inflammatory status. For instance:
- Elevated CRP can diagnose infection or inflammatory disease.
- Treatment response can be evaluated by monitoring CRP and other reactants.
- Specific proteins such as fibrinogen and homocysteine levels help in cardiovascular risk determination. – Detecting deficiencies (like AAT deficiency) aids in diagnosing genetic conditions.
- — Clinical Applications and Examples
- – Infection: Raised CRP and serum amyloid A indicate active viral or bacterial infection.
- – Autoimmune Diseases: Persistently raised CRP levels can indicate active rheumatic diseases.
- – Cardiovascular Disease: High fibrinogen and CRP levels are linked to a heightened risk for heart attacks.
- – Genetic Disorders: Low ceruloplasmin indicates Wilson’s disease; low AAT indicates risk of emphysema.
- — Reflections and Final Thoughts
- Acute-phase reactants are similar to the body’s early warning system, alerting clinicians to active inflammation or tissue damage. Being aware of which proteins react quickly and how their levels change assists in diagnosing, monitoring, and managing a wide range of diseases.
- Prompt for Reflection:
- Looking to your future practice as a healthcare practitioner, how might you use the measurement of these reactants in caring for patients? How would you interpret their levels in different clinical situations?
- — Further Reading and References
- – Gabay, C., & Kushner, I. (1999). Acute-phase proteins and other systemic responses to inflammation. New England Journal of Medicine, 340(6), 448–454.
- – Jaffe, E. S. (2010). Acute phase reactants and their clinical significance. Clinical Chemistry, 56(4), 503–510.
- – McDonald, J. C., & Hill, S. (2014). Laboratory evaluation of acute-phase proteins. American Journal of Clinical Pathology, 142(2), 161–170.
- – Henry, J. B. (2011). Clinical Diagnosis and Management by Laboratory Methods. 22nd Edition, Saunders.
- — Conclusion
- It is essential to understand acute-phase reactants for the interpretation of laboratory investigations of inflammation and infection. Knowing their functions, response times, and clinical relevance prepares future medical laboratory scientists and clinicians to make sound decisions and offer improved patient care.